

Sterility assurance monitoring is a vital component of your facility's overall quality assurance program. Sterility assurance products including biological indicators (BI) and chemical indicators (CI) provide you the confidence that the sterilizer is functioning properly and cycle conditions are adequate to produce medical devices that are ready and safe for patient use after reprocessing. Sterility assurance products are used for all sterilization modalities including steam, vaporized hydrogen peroxide (VHP), and ethylene oxide (EO). This article will focus on sterility assurance for steam and VHP sterilization.
Various industry governing bodies, such as the Association for the Advancement of Medical Instrumentation (AAMI), provide a range of guidance documents, recommendations, and standards for sterility assurance monitoring. The American National Standards Institute (ANSI) is the United States national standard body and all US standards and recommended practices with national recognition must be accepted by ANSI. Professional Associations like the International Association for Healthcare Central Service Material Management (IAHCSSM) provide education on best practices utilizing ANSI/AAMI standards and guidelines.
ANSI/AAMI ST79 – Comprehensive Guide
to Steam Sterilization and Sterility Assurance
in Health Care Facilities
The reprocessing of medical devices involves several steps. Facilities should follow accepted guidelines for cleaning, inspection and assembly, packaging, sterilization, transport and storage, in addition to maintaining utilities and environmental conditions required for proper functioning of equipment. With so many variables in the process, sterility assurance monitoring plays an important role in the overall quality assurance program to help verify and maintain the sterility of medical devices or instruments until it is used on a patient.
When manufacturer’s instructions for use (IFU) for reprocessing equipment and the medical device are followed, along with following Association for the Advancement of Medical Instrumentation (AAMI) recommendations for process monitoring, there is a high probability the instrument sets and devices are sterile.
ANSI/AAMI ST79 Comprehensive guide to steam sterilization and sterility assurance in health care facilities defines five processes in sterility assurance monitoring:
Qualification testing verifies the sterilizer’s performance before it is used. Qualification testing should be performed after installation or relocation and after sterilizer malfunctions, sterilization failures, or major repairs.

What tests are used for qualification testing?
Qualification testing consists of running three consecutive biological indicator challenge packs, also known as process challenge devices (PCD), with negative results to monitor the efficacy of the sterilizer. And then running three consecutive negative air removal tests, also known as Bowie-Dick tests or DART tests, to check for residual air that may be present during a cycle. The air removal test is only required for prevacuum sterilizers.
Routine monitoring confirms the steam sterilizer’s ability to remove residual air and provide lethality to highly resistant bacterial spores. Successful routine monitoring is a passing air removal test, passing CIs and negative results from BI tests.

What tests are used for routine monitoring?
An air removal test should be run in prevacuum sterilizers each day the sterilizer is used. According to ANSI/AAMI ST79, BI testing should be performed at least weekly, but best practice is running a BI test pack in every load for the highest level of patient care. Additionally, a Biological Indicator Process Challenge Device should be used in each load that contains implantable devices.
Load release requires evaluating all available monitors to determine if a specific cycle was successful. No one single sterility assurance product or indicator should be used to determine load release.
What monitors are used for load release?
Healthcare facilities use three types of monitors when deciding to release a load. The physical monitor, which is the cycle print-out, confirms all parameters of the sterilization cycle including sterilization time, temperature, and pressure were met. Chemical indicators, both external and internal, confirm the sterilization cycle was run and steam was able to penetrate the packaging. Biological indicators are also evaluated in loads that include BIs. If a BI is not added to the load, a CI PCD may be included and evaluated prior to load release.
Package release involves evaluating external and internal chemical indicators prior to the use of a package. These indicators are evaluated at the point-of-use.

What monitors are used for package release?
External chemical indicators are placed on the exterior of each package. They are used to differentiate between items that have been processed from those that have not.
Internal chemical indicators are placed within each package sterilized and confirm steam penetration into the package and that all critical parameters were met.
Product quality assurance testing verifies, by using the process as described in ANSI/AAMI ST79 section 13.9, the procedures in the manufacturer’s written IFU for cleaning, assembly, packaging and steam sterilization of devices, can be reproduced with the same results of a clean, dry, sterile device or set by the facility.
Sterility Assurance Monitoring for VHP Sterilization is similar to steam sterilization and is defined by ANSI/AAMI ST58.

Qualification testing for VHP sterilization verifies the sterilizer’s performance before it is used. Qualification testing should be performed after installation or relocation and after sterilizer malfunctions, sterilization failures, or major repairs. Unlike steam sterilization, qualification testing does not include the use of a Bowie-Dick or Air-Removal testing products.
Routine monitoring confirms the VHP sterilizers ability to provide lethality to highly resistant bacterial spores.
Load release for VHP sterilization still requires evaluating all available monitors to determine if a specific cycle was successful, just like in steam sterilization. Healthcare facilities use the same four types of monitors when deciding to release a load processed in VHP, as they do with Steam Sterilization. This includes physical monitors, chemical indicators, both external and internal, and biological indicators.
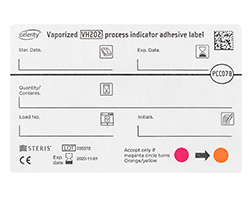
Package release for VHP sterilization is similar to steam sterilization. External chemical indicators are used to differentiate between items that have been processed from those that have not, while internal chemical indicators are placed within each package sterilized.

Biological indicators (BI) verify that the necessary conditions were met to kill a population of highly resistant non-pathogenic bacterial spores. The sterilization process uses spores identified as most resistant to a given sterilization process. The BI demonstrates the lethality of that sterilization cycle. Geobacillus stearothermophilus spores are primarily used in steam and vaporized hydrogen peroxide (VHP) biological indicators due to their high resistance to these sterilization processes (AAMI ST 58, AAMI ST79).

Chemical indicators (CI) are sterilization monitoring devices that respond to sterilization conditions with a chemical or physical change. Chemical indicators can help in the early detection of different sterilization failures such as:
AAMI identifies six types of chemical indicators, with each type having specific performance specifications that must be met. Learn more about the types of chemical indicators used in healthcare.
Documentation and record keeping are a critical part of the facility’s sterility assurance program. Accurate and complete record keeping is important for sterilization documentation. AAMI stresses the importance of record keeping for many reasons such as epidemiology purposes, sterilization activities, instruments tracking through patient use, implantable device sterilization, and maintenance and repair activity for all sterilizers.
Sterilization records may include:
There is no national standard for how long records need to be maintained. Always check with your state and local authorities, infection control, and hospital risk management or legal departments to determine record retention.

A sterile medical device is free from all viable microorganisms. The sterility of a product is defined by the probability of a single viable microorganism occurring on an item after sterilization. This probability is referred to as a sterility assurance level (SAL). The SAL is normally expressed as 10 n and is a quantitative value used to assure sterility assurance. A SAL of 10 6 means that there is less than or equal to one chance in a million that a single viable microorganism is present on a sterilized item (AAMI ST79).
A lower SAL indicates a greater assurance of sterility. While 100% assurance of sterility can never be reached the SAL for a sterile medical device should be reduced to very low numbers.
The Spaulding classification system divides medical instruments and equipment into three categories (critical, semi critical, and noncritical) based on the risk of infection from contamination on the item. For medical device sterilization, the most rigorous SAL should be used based on the ability of the product to function after sterilization while ensuring regulatory requirements are met for the specific device.
10 6 SAL or a SAL providing greater assurance of sterility is used for:
Examples of these types of medical devices include scalpels, surgical forceps, and implants.

Lisa Huber BA, CRCST, CIS, CHL, ACE, FCS, CQIA
Clinical Education Specialist
Lisa has been involved with developing CS education throughout her career. She has participated in the development of the IAHCSMM CS Technical Manual and Leadership Manual, she has presented locally, nationally, and internationally and has written several articles and lesson plans for professional publications. Lisa was President of IAHCSMM from 2009 to 2011.

Chasity Seymour BSHM, CST, CRCST, AGTS
Clinical Education Specialist
Chasity is a healthcare leader with over 13 years of experience in the Operating Room and Sterile Processing. Throughout her career she has transitioned into various leadership roles that include Surgical Technology Program Coordinator, SPD Manager, and Instrument Processing Regional Manager. In addition to articles for professional publications, Chastity has presented on the local as well as the national stage at the 2017 IAHCSMM Annual Conference.